COVID hospitalisations and deaths are rising faster than cases – but that doesn't mean more severe disease
- Written by Adrian Esterman, Professor of Biostatistics and Epidemiology, University of South Australia
Australia is currently in its third[1] Omicron wave (second if you live in Western Australia). This one is caused by the subvariants BA.4 and BA.5.
New variants gain an advantage[2] over previous variants by being able to spread more rapidly. This could be because they can replicate faster, are better able to latch onto human cells, or are better able to escape immunity.
Experts are worried[3] our health system will soon be overwhelmed, and then there is the potential loss of loved ones. At this point, the number of COVID cases is rising but still well short of the peak seen early this year. Yet hospitalisations and deaths are nearing previous peaks. What is going on?
Read more: How are Australia and NZ managing the rising COVID winter wave – and is either getting it right?[4]
A gentler curve
The first wave[5] of Omicron, caused by subvariant BA.1, began last November, with the epidemic curve rising sharply like a cliff face to about 100,000 cases a day nationally at its peak in early January.
The second wave, caused by Omicron BA.2, had a gentler curve, and peaked at the end of March with more than 60,000 cases per day.
The BA.4 and BA.5 curve is looking gentler still, with current daily case numbers at about 40,000. The peak is expected in August[6].
It is unclear why we are seeing these changes in successive Omicron waves, but it could be due to different levels of immunity in the population over time, along with changes in the genetic makeup of the subvariants.
Read more: Australia is heading for its third Omicron wave. Here's what to expect from BA.4 and BA.5[7]
People admitted to hospital with COVID
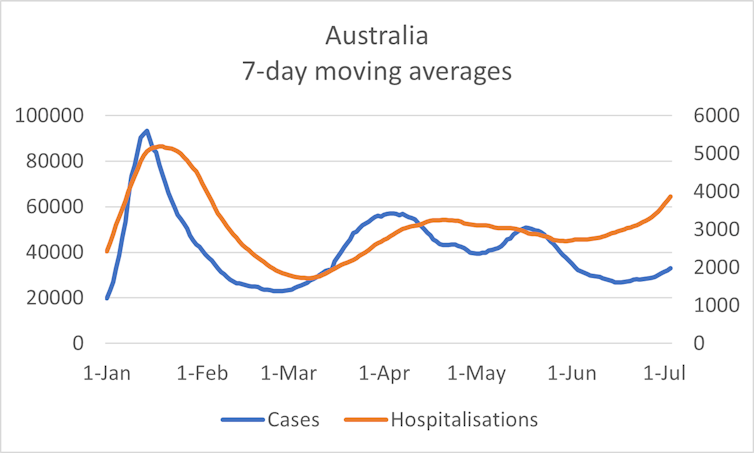
The graph below plots cases in Australia versus hospitalisations this year.
As hospitalisations usually occur[8] on average one week after diagnosis, the cases have been lagged by seven days. In other words, cases on January 1 2022 are plotted against hospitalisations on January 8 2022. However, it should be noted this diagnosis-to-hospitalisation time is from 2020, and might be different now.
Clearly, since the beginning of June, hospitalisations have been increasing at a faster rate than case numbers. But does this necessarily mean BA.4 and BA.5 are causing a more severe disease?
ICU admissions
Hospitalisations are a bit difficult to interpret as there is no agreed definition of what a hospitalisation is. For example, do you include hospital in the home, or patients diagnosed after they have been admitted for something else?
Admissions to hospital intensive care units (ICUs) are much easier to interpret. If someone is admitted to ICU, they are critically ill.
The chart below shows ICU admissions as a percentage of hospitalisations. The average time[9] from being admitted to ICU after admission to hospital is one day, so no lagging has been applied here (with the same caveat about 2020 data as before).
Clearly, since the beginning of the year there has been a declining proportion of patients admitted to the ICU, and it has now levelled out at about 3.2%.
However, there are potentially many factors to consider. First, there are only a limited number of ICU beds, which could keep ICU numbers for COVID artificially low.
Lower numbers of COVID-19 patients in ICU could simply be a result of increasing deaths in ICU.
At the same time, better hospital treatment with antivirals such as Paxlovid, Lagevrio and Remdesivir, and monoclonal antibodies like Regdanvimab could be keeping hospitalised patients out of the ICU.
Read more: COVID drugs in Australia: what's available and how to get them[10]
The winter effect
Winter[11] sees an increase in respiratory diseases such as pneumonia, influenza and now COVID, as well as heart diseases.
Many people who are already in hospital may also have COVID, or may get COVID in hospital, but it’s not the primary reason they are there, and this has likely increased during the current winter season.
Cases that are undiagnosed or not reported
The number of diagnosed daily cases is only an estimate, with the true number of cases likely several times greater[12]. This is because:
-
asymptomatic people don’t usually test themselves without a good reason
-
those with symptoms might think it is just a common cold and not test themselves, especially in winter
-
those who test themselves with a rapid antigen test (RAT) have a reasonable chance[13] of a false negative result, especially in the first 48 hours
-
some people who test positive on a RAT might not report the result to authorities
-
the definition of a reinfection has changed from 3 months to 28 days after the initial infection. This means many reinfections would have been missed until now.
In other words, the increasing number of hospitalisations we are seeing might be due to more undiagnosed cases in the community in the past few weeks. This week, the South Australian chief health officer said[14] sewage testing indicated there were likely many more COVID cases than those being reported.
Lives lost
Finally, the graph below plots cases in Australia versus deaths. As deaths likely occur on average[15] two weeks after diagnosis, the cases have been lagged by 14 days (this estimate is based on 2021 data). In other words, cases on January 1 2022 are plotted against hospitalisations on January 15 2022.
COVID deaths are now going up at a faster rate than cases. Again, this could simply be because there are more people in hospital with COVID plus other illnesses because of winter, leading to a higher death rate. This could also be why we are seeing more deaths now.
So, a discussion about whether the current wave caused by BA.4 and BA.5 is leading to more severe disease is complicated. Even though the charts show hospitalisations and deaths increasing faster than case numbers, this could be the winter effect, under-diagnosis or under-reporting – or a combination of these factors.
Regardless, we do know our health system is under increasing pressure[16], with not only more patients, but also increasing numbers of doctors, nurses and ambos off sick with COVID.
The best thing we can do to try and relieve this pressure is protect ourselves and others. This is not difficult. We simply need to make sure we are up-to-date with our booster shots, and wear a face mask when out and about.
Read more: When can I get my next COVID booster or fourth dose? What if I've recently had COVID? Can I get my flu shot at the same time?[17]
References
- ^ third (theconversation.com)
- ^ advantage (jamanetwork.com)
- ^ worried (www.theguardian.com)
- ^ How are Australia and NZ managing the rising COVID winter wave – and is either getting it right? (theconversation.com)
- ^ first wave (ourworldindata.org)
- ^ August (www.news.com.au)
- ^ Australia is heading for its third Omicron wave. Here's what to expect from BA.4 and BA.5 (theconversation.com)
- ^ occur (www.mja.com.au)
- ^ time (www.mja.com.au)
- ^ COVID drugs in Australia: what's available and how to get them (theconversation.com)
- ^ Winter (www.aihw.gov.au)
- ^ likely several times greater (www.afr.com)
- ^ chance (journals.asm.org)
- ^ said (indaily.com.au)
- ^ average (www.medrxiv.org)
- ^ pressure (www.abc.net.au)
- ^ When can I get my next COVID booster or fourth dose? What if I've recently had COVID? Can I get my flu shot at the same time? (theconversation.com)

















