Masks are 'strongly suggested' by health authorities as the winter COVID wave hits. Here's how effective they are
- Written by Thea van de Mortel, Professor, Nursing and Deputy Head (Learning & Teaching), School of Nursing and Midwifery, Griffith University
Health departments are predicting another COVID surge[1] related, in part, to more easily transmitted new variants and waning immunity.
Given COVID cases are rising and likely underestimated, Chief Medical Officer Paul Kelly has strongly suggested[2] people wear masks in indoor spaces.
So it’s important to get across how effective they are and which type to choose. Is it worth dusting off last year’s cloth masks, using a surgical mask, or going out to buy some N95 respirators to wear over the coming weeks?
Read more: 6 steps to making a COVID plan, before you get sick[3]
COVID spread and the effects of winter
The SARS-CoV-2 virus (which causes COVID) spreads mainly through breathing in contaminated droplets or aerosols[4] (tiny particles that are left when fine droplets dry out) released into the air[5] when an infectious person breathes, talks, laughs, shouts, coughs or sneezes. This can happen even when they don’t have any symptoms.
Larger droplets fall to the ground quickly, so distancing yourself from others gives you some protection. Aerosols, though, can hang in the air for hours and travel all around a room.
So you can be infected by aerosols indoors even at a distance from an infectious person or after they have left the room.
COVID case numbers tend to increase during winter. This may be because:
the virus remains viable (able to cause an infection) for longer in cool and less humid conditions[6]
we tend to remain indoors when it’s cold, and sharing indoor spaces[7] with others increases the risk of contracting COVID.
Read more: COVID hospitalisations and deaths are rising faster than cases – but that doesn't mean more severe disease[8]
Which indoor spaces are the most risky?
The most risky indoor settings are:
places where people are talking loudly[9], laughing, singing or shouting, because more[10] droplets and aerosols are released
rooms where ventilation is poor, as the contaminated particles are not being quickly removed
spaces that are crowded[11] or where you are exposed for a longer period[12], as the risk goes up with extended contact.
In other words, spending two minutes in a small shop with an open door and one other person present is less risky than sitting in a crowded indoor bar for hours where everyone is talking loudly to be heard over the background noise.
What can I do?
Wearing a mask or respirator can protect you and others in the community from COVID infection. Some people are at greater risk of severe illness due to old age or poorly functioning immune systems.
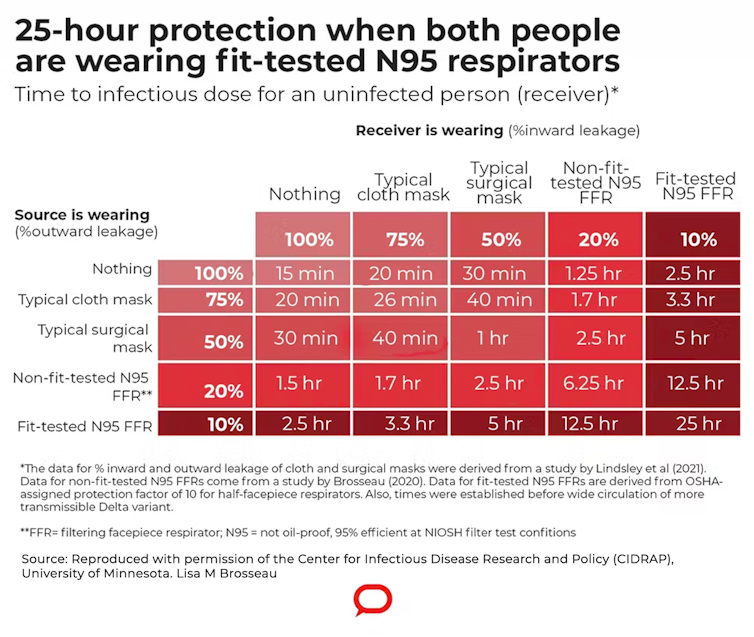
As the table below[13] shows, when both the infected and uninfected person wear a mask or respirator, the protection is greater than if just one of them wears one.
References
- ^ COVID surge (www.abc.net.au)
- ^ suggested (www.afr.com)
- ^ 6 steps to making a COVID plan, before you get sick (theconversation.com)
- ^ contaminated droplets or aerosols (www.cdc.gov)
- ^ released into the air (first10em.com)
- ^ cool and less humid conditions (www-ncbi-nlm-nih-gov.libraryproxy.griffith.edu.au)
- ^ indoor spaces (www.ncbi.nlm.nih.gov)
- ^ COVID hospitalisations and deaths are rising faster than cases – but that doesn't mean more severe disease (theconversation.com)
- ^ talking loudly (www.nature.com)
- ^ more (www.nature.com)
- ^ crowded (www.epa.gov)
- ^ longer period (www.epa.gov)
- ^ table below (www.cidrap.umn.edu)
- ^ CC BY-ND (creativecommons.org)
- ^ standard (www.fda.gov)
- ^ source control (www.fda.gov)
- ^ meta-analysis (www.ncbi.nlm.nih.gov)
- ^ community (www.ncbi.nlm.nih.gov)
- ^ Time to upgrade from cloth and surgical masks to respirators? Your questions answered (theconversation.com)
















