80% vaccination won't get us herd immunity, but it could mean safely opening international borders
- Written by Tony Blakely, Professor of Epidemiology, Population Interventions Unit, Centre for Epidemiology and Biostatistics, Melbourne School of Population and Global Health, The University of Melbourne
The first phase of Prime Minister Scott Morrison’s four-stage “pathway out of the COVID-19 pandemic[1]”, announced on Friday, focuses on vaccinating as many Australians as possible, while halving the cap on international arrivals.
Morrison expects phase one, which we’re currently in, to be in place until 2022. But he said it’s hard to give a definitive answer on when we’ll get to phase two because vaccination targets have not yet been set. He’s waiting for the modelling.
Phase two of Morrison’s plan is a move back to the current levels of international arrivals, and a separate cap for vaccinated travellers. Phase three sees Australians able to travel abroad and no cap on returnees.
We are undertaking our own detailed modelling of border openings and while we’re yet to release our models, we can still arrive at fairly solid conclusions now. We’re basing these on the theory that Australia could substantially open its borders in the second quarter of 2022 with quarantine-free travel from many (but not all) countries.
The key trick, though, is to not think of vaccination as the only intervention. It is vaccination — together with three other measures: ongoing aggressive contact tracing, mask-wearing in high-risk settings and some physical distancing — that will make it safe to open.
Put another way, even when we immunise all Australians who want to be protected against COVID-19, we’re unlikely to achieve herd immunity through vaccination alone.
Vaccination targets
Modelling performed by the University of Sydney[2], the Burnett Institute[3] and previously by us all point to the reality that opening the borders before about two-thirds of the population is vaccinated (in the absence of strong additional methods) could cause considerable illness and death.
So it seems unethical to substantially open the borders until everyone has had a fair opportunity to get vaccinated. All going well, this should occur sometime in the second quarter of 2022.
This would, however, be dependent on children also having the opportunity to be vaccinated. While other countries have started vaccinating children, Australia has yet to approve this use.
Vaccination alone won’t get us herd immunity
Some vaccination programs alone can achieve herd immunity, or resilience, meaning the virus won’t spread easily and exponentially, in the absence of masks, contact tracing and the other measures we have used during the pandemic.
But given the Delta variant means an average infected person infects five others without any other measures in place, and given vaccines are not perfect, Australia would need 90% of adults and children vaccinated to achieve herd immunity (through vaccination alone). This is unlikely.
There will be some waning in vaccine immunity over time, and new variants for which Pfizer and AstraZeneca are less effective. However, even with 100% of the population vaccinated, herd immunity may not be achieved by vaccination alone until booster vaccines become available.
 We need as many Australians to get vaccinated as possible, but we’ll still need other measures to keep a lid on outbreaks.
CDC/Unsplash[4]
We need as many Australians to get vaccinated as possible, but we’ll still need other measures to keep a lid on outbreaks.
CDC/Unsplash[4]
How did we get to 90%?
The Delta variant has an R0 (the number of people one infected person on average infects) of about 5.0[5] under pre-COVID-19 ways of living. This is twice that of the original Wuhan virus which had an R0 about 2.5.
For an R0 of 5.0, theoretically, 80% of the population have to be immune — not just vaccinated — for virus transmission not to take off.
But the actual vaccine coverage required is higher, as the vaccines aren’t 100% effective at stopping any infection. And even though a person has been vaccinated, it doesn’t mean they’re always immune from the virus, as the person may not develop a strong immune response.
Vaccination with two doses of Pfizer among adults aged 16-60 years old is likely about 80% successful[6] at stopping any Delta infection. For those 60 or older, the effectiveness of AstraZeneca at reducing the risk of any infection is less: about 60%[7] against the Delta virus.
Read more: Should I get my second AstraZeneca dose? Yes, it almost doubles your protection against Delta[8]
Over half, 58%, of the population are aged 16-59, and 23% of the population are aged 60-plus. So for 80% vaccination coverage of adults, the estimated percentage of the population who are immune is 48% — well short of the 80% herd immunity threshold.
For those still at risk of getting infected after either Pfizer or AstraZeneca vaccination, they are 50% less likely[9] to transmit it. So the 16% of the population who were vaccinated but can still get infected are half as likely to pass it on.
The remaining 36% of the population are fully susceptible (20% of adults, and all children).
Extending this maths, we need about 90% of everyone (children and adults) to be vaccinated to achieve herd immunity. This is unlikely to happen.
What’s our alternative?
Using both the above theory, and what we have seen so far in our modelling, we can outline scenarios going forward:
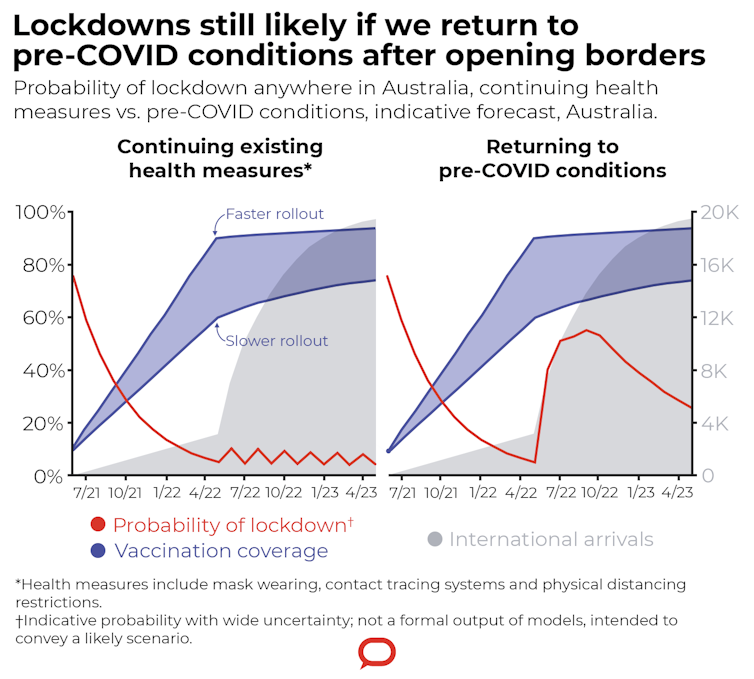 Author modelling/The Conversation, CC BY-ND[10]
From now until about April 2022, we propose we vaccinate as many people as possible and retain the goal of zero community transmission. Eliminating the virus after each outbreak will get easier with increasing vaccine coverage. And the probability each month of a lockdown somewhere in Australia will diminish.
This phase in our modelling is similar to the government’s first phase.
Back to our scenario: in early-to-mid 2022, we propose some modest opening of borders, through travel bubbles to other countries with virtually no community transmission, such as China and Singapore.
This is a divergence from the government’s second phase.
By mid-2022, we could allow many more countries to have quarantine-free travel to Australia, and arrivals might jump to something like half the volume pre-COVID-19.
However, people from high-risk countries — with a peak in infection, or a new variant of concern — would still have to go through 14-day (or modified) quarantine, in Howard Springs or purpose-built facilities, rather than hotel quarantine.
Then we have two choices.
If we open up to pre-COVID settings — with no contact tracing, no masks, no physical distancing — there will be repeated and serious outbreaks requiring lockdowns.
We might see enough natural infection to top-off the vaccination-induced immunity to get us to something like herd immunity. But the numbers are frightening: we may need about a fifth of us to acquire natural infection. That is five million Australians infected with substantial illness and death.
Read more:
The 'herd immunity' route to fighting coronavirus is unethical and potentially dangerous[11]
Thankfully, we have another choice: accept that some restrictions and public health measures need to continue beyond mid-2022 to complement vaccination.
As noted in the graph above, there is still a lot of uncertainty about how we open up the borders. We, and other groups, are actively modelling these options to more fully articulate and quantify pathways out.
The good news is even though herd immunity through vaccination alone is no longer a realistic option, there is an alternative path out through high vaccine coverage augmented by ongoing contact tracing, mask-wearing and physical distancing.
Put another way, 80% vaccination of adults pulls the effective reproductive rate down from 5.0 to 2.2, which is not enough to stop exponential spread. But a mix of mask-wearing, contact tracing and physical distancing will be enough to pull the effective reproductive rate to less than 1.0 — low enough to halt the spread of COVID-19.
Author modelling/The Conversation, CC BY-ND[10]
From now until about April 2022, we propose we vaccinate as many people as possible and retain the goal of zero community transmission. Eliminating the virus after each outbreak will get easier with increasing vaccine coverage. And the probability each month of a lockdown somewhere in Australia will diminish.
This phase in our modelling is similar to the government’s first phase.
Back to our scenario: in early-to-mid 2022, we propose some modest opening of borders, through travel bubbles to other countries with virtually no community transmission, such as China and Singapore.
This is a divergence from the government’s second phase.
By mid-2022, we could allow many more countries to have quarantine-free travel to Australia, and arrivals might jump to something like half the volume pre-COVID-19.
However, people from high-risk countries — with a peak in infection, or a new variant of concern — would still have to go through 14-day (or modified) quarantine, in Howard Springs or purpose-built facilities, rather than hotel quarantine.
Then we have two choices.
If we open up to pre-COVID settings — with no contact tracing, no masks, no physical distancing — there will be repeated and serious outbreaks requiring lockdowns.
We might see enough natural infection to top-off the vaccination-induced immunity to get us to something like herd immunity. But the numbers are frightening: we may need about a fifth of us to acquire natural infection. That is five million Australians infected with substantial illness and death.
Read more:
The 'herd immunity' route to fighting coronavirus is unethical and potentially dangerous[11]
Thankfully, we have another choice: accept that some restrictions and public health measures need to continue beyond mid-2022 to complement vaccination.
As noted in the graph above, there is still a lot of uncertainty about how we open up the borders. We, and other groups, are actively modelling these options to more fully articulate and quantify pathways out.
The good news is even though herd immunity through vaccination alone is no longer a realistic option, there is an alternative path out through high vaccine coverage augmented by ongoing contact tracing, mask-wearing and physical distancing.
Put another way, 80% vaccination of adults pulls the effective reproductive rate down from 5.0 to 2.2, which is not enough to stop exponential spread. But a mix of mask-wearing, contact tracing and physical distancing will be enough to pull the effective reproductive rate to less than 1.0 — low enough to halt the spread of COVID-19.
References
- ^ pathway out of the COVID-19 pandemic (www.theguardian.com)
- ^ University of Sydney (arxiv.org)
- ^ Burnett Institute (www.burnet.edu.au)
- ^ CDC/Unsplash (unsplash.com)
- ^ about 5.0 (www.abc.net.au)
- ^ about 80% successful (www.thelancet.com)
- ^ about 60% (www.medrxiv.org)
- ^ Should I get my second AstraZeneca dose? Yes, it almost doubles your protection against Delta (theconversation.com)
- ^ 50% less likely (www.nejm.org)
- ^ CC BY-ND (creativecommons.org)
- ^ The 'herd immunity' route to fighting coronavirus is unethical and potentially dangerous (theconversation.com)

















